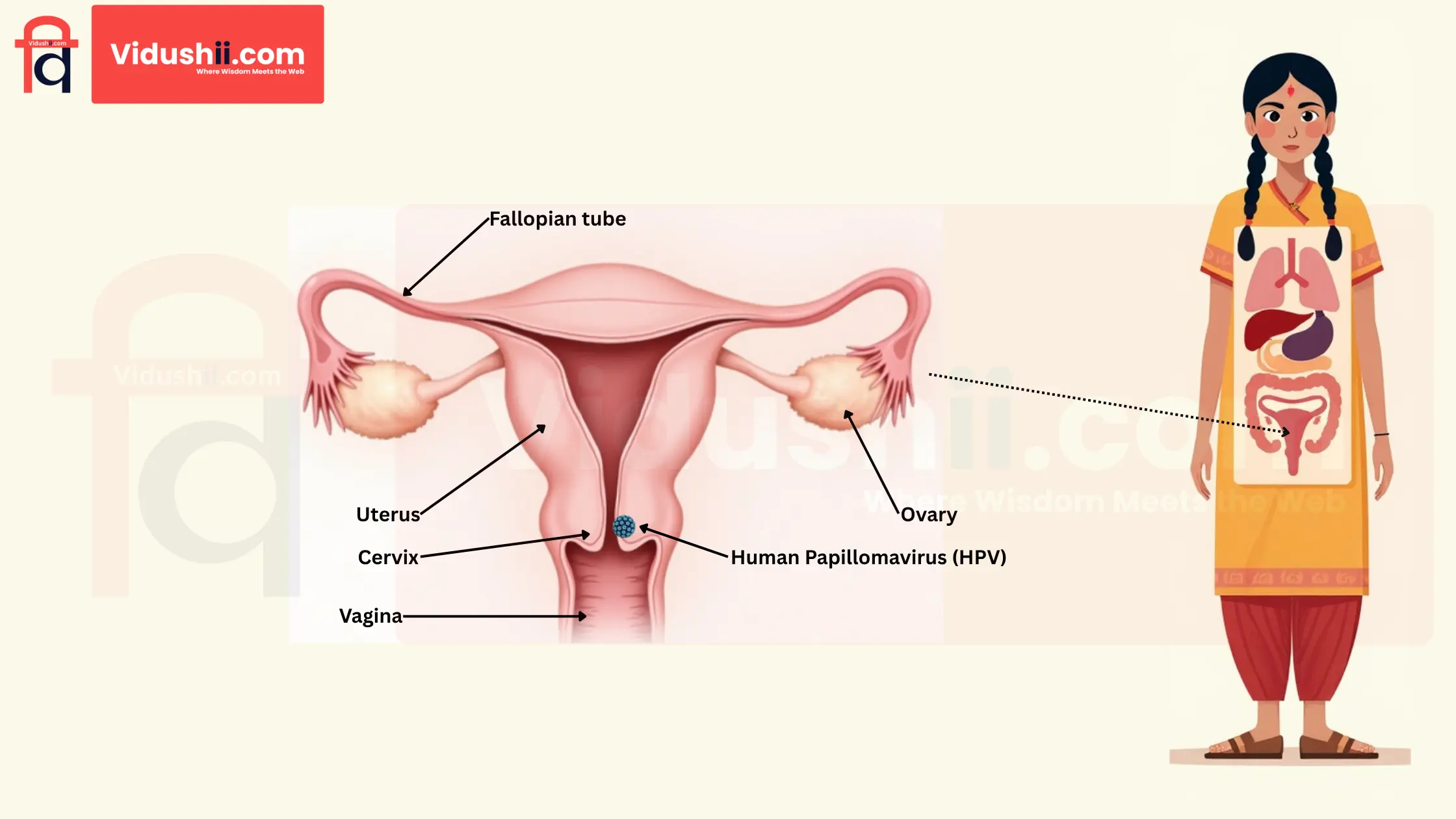
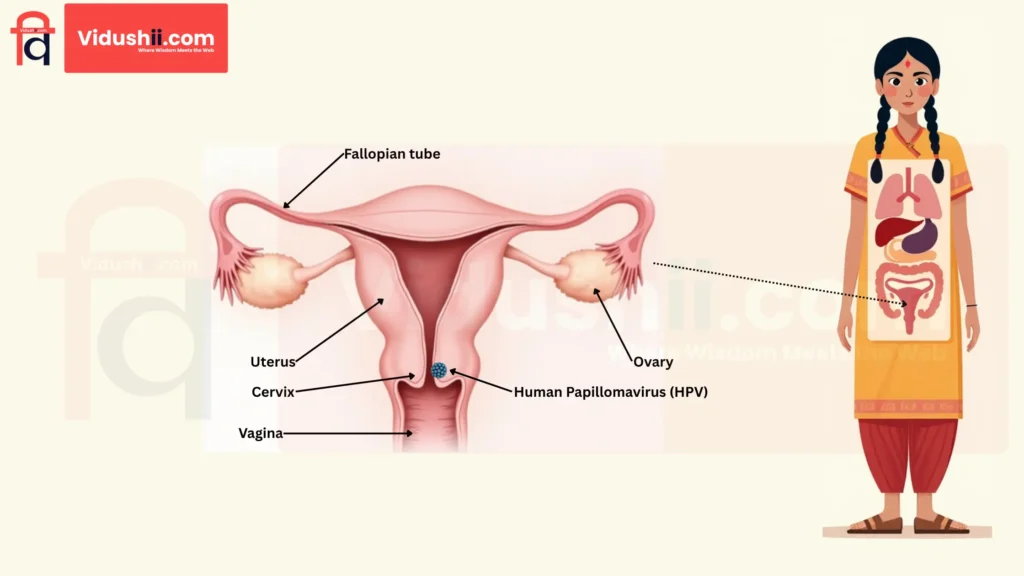
Cervical cancer is the most common cancer in women, and it’s mainly caused by a virus called Human Papillomavirus (HPV). High-risk variants of HPV ( 16 and 18 ) can lead to cervical Intraepithelial Lesions ( abnormal cell growths that occur within the lining (epithelium) of certain organs ), which can eventually progress to cervical cancer. In India and other developed countries, the VIA test, the HPV DNA test and the Pap Smear test (also known as the Papanicolaou Smear Test) are involved in screening and early detection. HPV testing identifies exposure to low and high-risk HPV, while the Pap smear identifies abnormal cytology.
According to researchers, Cervical Cancer is 100% preventable. Awareness, Prevention and Early Detection are the most effective ways to reduce mortality from cervical cancer.
How Many Types Of Cervical Cancer Are There?
Cervical cancer is named after the type of cell in which the cancer originated. There are two main types:
- Squamous cell carcinoma: Up to 90% of cervical cancers are squamous cell carcinomas. This cancer develops from cells in the ectocervix.
- Adenocarcinoma: Adenocarcinomas develop in the glandular cells of the endocervix. Clear cell adenocarcinoma, also called mesonephroma or clear cell carcinoma, is a rare type of cancer of the cervix.
Cervical cancer sometimes consists of both adenocarcinoma and squamous cell carcinoma. This is called adenosquamous carcinoma or mixed carcinoma. There is a very rare chance that cancer develops in other cells in the cervix.
What causes cervical cancer?
Nearly all cervical cancers are caused by high-risk types of human papillomavirus (HPV), which involve long-term (persistent) infection. HPV 16 and HPV 18 cause 70% of cervical cancers worldwide.
The risk of becoming infected with high-risk types of HPV is higher in people who become sexually active at a younger age, especially before age 18, or who have multiple sexual partners.
HPV occurs in almost all sexually active people. Most HPV infections clear up on their own within a year or two as the immune system controls the infection. These minor infections do not typically develop into cancer. When a high-risk HPV infection persists for years, it can cause changes in the cells of the cervix, which may lead to a precancerous lesion. Cervical cancer can eventually develop on the cervix if a precancerous lesion is not detected and removed.
Factors that increase the risk of developing Cervical cancer from HPV infection.
- Weak Immune System: Having a weak immune system can reduce the body’s ability to fight off HPV infection. People who have a weakened immune system are more likely to develop an HPV infection and develop into cancer.
- Smoking or Passive Smoking or Secondhand Smoke: The risk of cervical cancer increases in people who smoke or breathe secondhand smoke.
- Contraceptive Use & Pregnancies: An increased risk of cervical cancer is associated with using contraceptives (birth control pills) and more frequent pregnancies.
- DES exposure: DES exposure is a rare cause of cervical cancer. Between 1940 and 1971, women were given a synthetic hormone called diethylstilbestrol (DES) to prevent miscarriage. Women who took DES during pregnancy have a higher risk of developing a rare cervical cancer.
- More Risk Factors:
- Genetic factors
- Low socio-economic status
- Multiple sexual partners
- Negligence in weight management
- Human Immunodeficiency Virus
Preventive measures for cervical cancer.
- Quit smoking: Quitting smoking boosts the immune system and helps prevent cervical cancer by reducing harmful toxins that can damage cervical cells.
- Practising safe sex: Practising safer sex (This includes using condoms, limiting the number of sexual partners, getting tested regularly for STIs, and open communication with partners about sexual health) can reduce the risk of HPV transmission, the main cause of cervical cancer, by minimising exposure to the virus.
- Stay in shape: Staying in shape boosts the immune system and maintains hormonal balance, which helps prevent cervical cancer, increasing the body’s ability to fight HPV infection.
- Keep an Eye on symptoms: Keeping an eye on the symptoms helps prevent cervical cancer, allowing early detection of abnormal changes and timely diagnosis and treatment.
- Do not ignore family history: Being aware of your family history helps identify genetic risks early, allowing for screening and prevention of cervical cancer.
- Eat foods that nourish the cervix: A diet rich in vitamins A, C and folate keeps the cervix healthy and reduces the risk of changes in cancer cells.
- Get regular checkups: Regular checkups, including VIA, Pap smears, and HPV DNA tests, can detect early changes in cervical cells, which can prevent cancer before it develops.
- Strengthen the immune system: A strong immune system helps fight HPV infection naturally, reducing the chances of cervical cell abnormalities that can lead to cancer.
- HPV vaccination: The HPV vaccine is an effective preventive because it protects against high-risk virus strains that cause most cervical cancer cases.WHO recommends the following measures according to its position on the HPV vaccine in December 2022:
- A 1 or 2-dose schedule for girls aged 9 to 14 years
- A 1 or 2-dose schedule for girls and women aged 15 to 20 years
- Women over 21 years of age should receive two doses at an interval of 6 months.
For those who are immunocompromised and/or HIV-infected, at least 2 doses, and when possible, 3 doses, are still required.
Consulting your doctor/gynec befor taking HPV vaccine is mandatory.
What are the Symptoms of cervical cancer?
- Abnormal Vaginal discharge: Irregular vaginal discharge may be a sign of infection or abnormalities in the cervix, which need medical attention.
- Loss of bladder control: Sudden incontinence may be a sign of pelvic pressure from a growing cervical tumour.
- Pelvic pain: Regular pelvic pain may be the first sign of a tumour or inflammation in the cervix, which leads to cervical cancer.
- Pain during sex: Irritation or sores of the cervix may cause discomfort during intercourse.
- Heavy and long menstrual cycles: Long or heavy bleeding may indicate changes in cervical cells or a hormonal imbalance.
- Abnormal bleeding, between periods, after sex or menopause: Irregular bleeding is a big sign of cervical cancer.
- Discomfort during urination: Discomfort during urination is also a symptom.
- Unexplained weight loss: Unexplained weight loss may be a symptom of cervical cancer.
- Persistent fatigue: Regular fatigue can also be a symptom of cervical cancer.
- Joint pain: Joint pain may be a symptom of cervical cancer.
What is Cervical Cancer Screening?
The examination of the cervix before any symptoms appear is known as Screening. Screening is an important part of prevention for cervical cancer.
There are 3 types of screening available.
- VIA Test (Visual Inspection with Acetic Acid): Every year.
- Pap Smear Test (Papanicolaou Smear Test): Every 3 years.
- HPV DNA Test (Human Papillomavirus Deoxyribonucleic Acid test): Every 5 years.
- HPV/Pap co-test (An HPV Pap co-test combines two cervical cancer screening methods: the Pap test, which checks for abnormal cell changes, and the HPV test, which detects the presence of human papillomavirus): Every 5 years
When to get screened for cervical cancer
- Women’s age should be between 30 to 65 years.
- 5 days after your period stops.
- Do not use birth-control jellies or foams, tampons, other vaginal creams, lubricants or moisturisers, or any vaginal medicines for up to 7 days before the test.
- Not using a douche (Vaginal wash) for 2 to 3 days before the test.
- Do not perform intercourse for 2 days before the test.
According to Final Recommendation Statement | Cervical Cancer: Screening August 21, 2018: For women of Age 21-29 years USPSTF recommends getting your first Pap test at age 21, followed by Pap testing every 3 years. Even if you are sexually active, you do not need a Pap test before age 21.
For women of Age 66 and older no screening needed if a series of prior tests were normal, but if you feel any symptoms more then 7 days then consult your Doctor/gynecologist.
If you have any advice or see any errors in this article, please let us know. We’ll happily address any issues and improve based on your input.
Email Us: info@vidushii.com